50 year old male, with complaints of shortness of breath and cough with sputum , distension of abdomen.
Unit II admission on 02/02/2021
DR. AMULYA ( INTERN)
DR. YAMINI ( INTERN)
DR. SURYA PRADEEP ( INTERN)
DR. ASHA KIRAN ( INTERN)
DR. JAYANTH ( INTERN)
DR. VAMSHI ( INTERN)
DR. ISMAIL (INTERN)
DR. PRADEEP ( PG 1st YEAR)
DR. NIKITHA ( PG 2nd YEAR)
DR. SUFIYA ( PG 3rd YEAR)
DR. SATISH ( PG 3rd YEAR)
Faculty : DR. VIJAYALAXMI
This is an online E log book to discuss our patient's de-identified health data shared after taking his/her/guardian's signed informed consent.
Here we discuss our individual patient's problems through series of inputs from available global online community of experts with an aim to solve those patient's clinical problems with collective current best evidence based inputs.
This E log book also reflects my patient-centered online learning portfolio and your valuable inputs on the comment box is welcome.
Here is a case I have seen:
50 year old male,waiter in hotel by occupation,came to casualty with complaints of SOB on exertion,distension of abdomen since 1month.
Cough since 6months,productive,white colour sputum,evening rise of temperature present,no history of weightloss
Facial puffiness on and off since 3 months
Increased frequency of micturition since 3 months.
HOPI :- Patient was apparently asymptomatic 10 years back, when he developed SOB on exertion and used medication , which increased on exposure to cold( seasonal variation present). The SOB increased from 20 days , progressed to even at rest and talking . He gives history of using inhalers since past 2 years which weren't prescribed by any doctor.History of fever which was on and off with an evening rise of temperature No history of orthopnea, PND.
Abdominal distension since 3 months. No history of pedal edema, no history diarrhoea and constipation. No history of vomitings or nausea, pain abdomen, no hemetemesis
Cough with sputum since 3 months. History of wheeze present. Sputum , clear in color and scanty in quantity non foul smelling , no hemoptysis.
Increased frequency of micturation. Not associated with burning, urgency, dot and line pattern. There is no difficulty initiating stream of urine. No history of incontinence.
Non hypertensive,non diabetic
Smoker and alcoholic since 20yrs
He is taking betamethasone 2 to 3 tablets/day since 1year,(given by outside doctor,and he continued to take medication whenever he had SOB)
Examination at time of admission:-
Patient conscious,coherent
Afebrile
Bp:120/80mmhg
PR: 84bpm
RR: 29/min
Spo2 91@room air
GRBS 312 mg/dl
No pedal edema,no facial puffiness
Abdomen distended
Clubbing+
Icterus mild+
Buffalo hump present and acanthosis nigrans
CVS :- S1 S2 heard
RS :- BAE present.
On auscultation fine crepts in right and left ISA , Bilateral IAA, and mammary area and B/L wheeze.
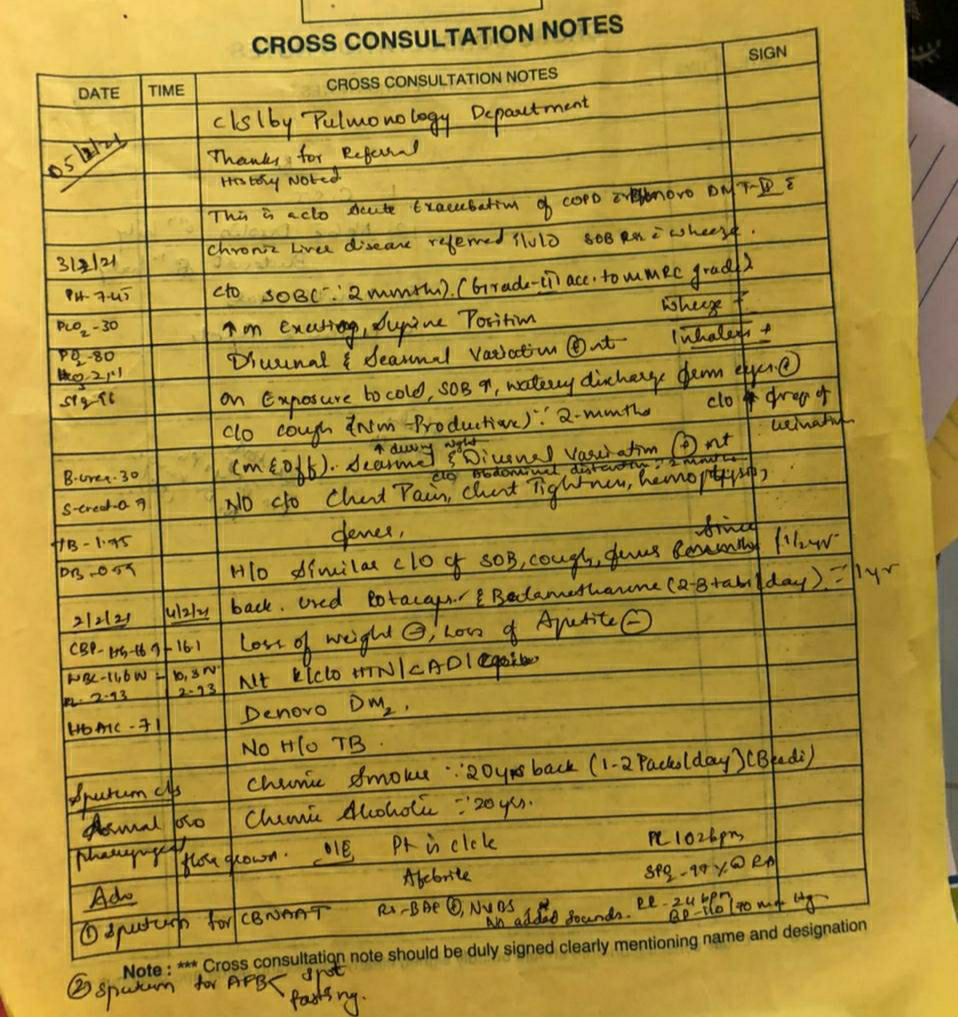
Update of 05-02-2021
S - subjectively cough hasn't subsidised and oxygen requirement varying
O - wheeze reduced to only being heard on the right side
Update of 07-02-2021
Srinu
S- Cough present during inspiration
O- Pt c/c/c
Afebrile
BP-140/100mmhg
PR-77bpm
RR-20cpm
Spo2-98% on RA
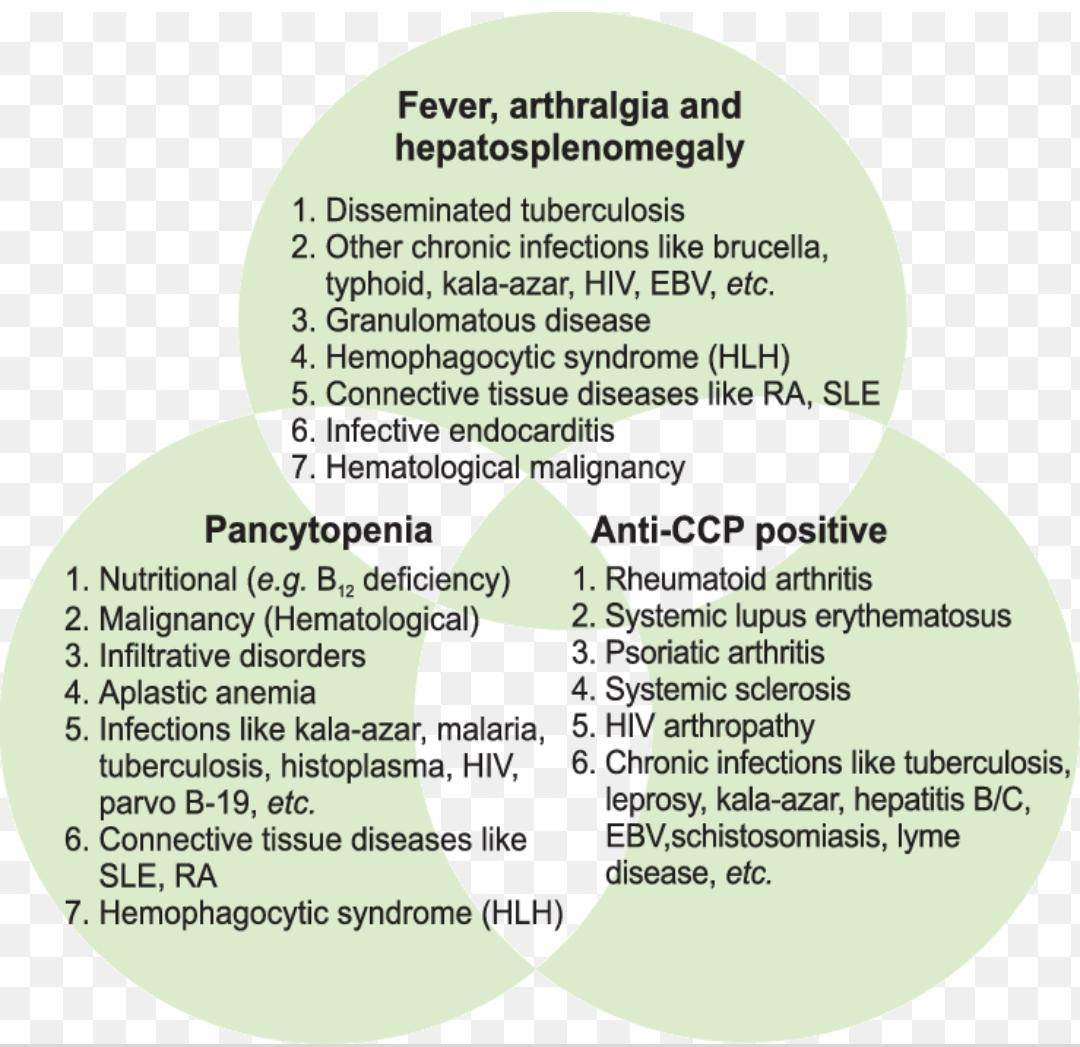
A- Acute exacerbation of COPD secondary to ?kochs with chronic liver disease with denovo DM-II (secondary to steroids)
Diagnosis: Acute exacerbation of copd
? Pulm Koch's
? Denovo detected DM
Or? secondary to steroid intake
Treatment on day of admission :-
1.) Propped up position
2.) Inj Augmentin 1.25 mg IV BD
3.) Inj Pan 40 mg IV OD
4.) Nebulization with 2 respules of salbutamol 8th hourly and budecort 12th hourly.
5.) Oxygenation to maintain SpO2 above 90%
6.) GRBS 6th hourly
7.) BP, temp, PR, SpO2 charting 4th hourly
8.) I/O charting
9.) Inj Lasix 20 mg IV OD if SBP more than 140mm Hg
10.) Inj Vitamin K 10 mg OD
11.) Syp Lactulose 15 ml PO TID.
12.) Inj Deriphyllin 1amp IV OD
13.) Inj hydrocortisone 100 mg IV OD
14.) Inj HAI SC 6IU - 6IU - 4IU
Provisional diagnosis Acute exacerbation of COPD 2° to pneumonia with chronic liver disease with denovo DM -2 (2° to steroids )
From 5-02-2021
1.) Head end elevation
2.) Inj Augmentin 1.25 mg IV BD
3.) Inj Pan 40 mg IV OD
4.) Nebulization with 2 respules of salbutamol 8th hourly and budecort 12th hourly.
5.) GRBS 6th hourly
6.) Inj Human Mixtard SC 30 IU - 15IU
7.) T. Metformin 500 mg BD
8.) Syp. Grillinctus 15ml PO TID
9.) Inj Deriphyllin 1amp IV OD
10.) Inj hydrocortisone 100 mg IV OD
11.)T. Montelucast -LC BD